Other Services and Specialties

Endodontics
What is endodontics?
Endodontics also known as root canal treatments, consists of the total extraction of the dental pulp (interior part of the tooth where the nerve and blood vessels are located) it presents inflammation, infection or necrosis (death) due to a deep dental cavity, trauma, abrasion, etc. Endodontics is performed with the aim of cleaning the tooth and avoiding its extraction.
Signs of an affected pulp
Physical symptoms usually appear when the problem is advanced. Symptoms can include dental sensitivity without the need for a direct stimulus, spontaneous and stabbing pain, change of color in the tooth (if there has been nerve involvement), inflammation of the gums around the affected tooth, and in extreme cases, abscesses with pus and halitosis, among others.
Technology for root canal treatment
In our clinic, we have highly qualified endodontists and state-of-the-art equipment for the successful completion of root canal treatment. The endodontist will use a dental microscope to observe, in detail, the area to work on. This will allow them to locate the canals easily and precisely, make airtight seals, locate fractures, cavities, supernumerary canals, etc.
To guarantee the success of a root canal treatment, it is very important to monitor the procedure step by step. How can we do this monitoring? We have a portable endodontic radiography system, which allows us to instantly obtain high-definition X-ray images of the root canal process, exposing the patient to 80% less radiation than with a conventional X-ray.
Periodontics
What is periodontics?
Periodontics is the specialty of dentistry that is responsible for the treatment of diseases of the gums and alveolar bone, including periodontitis and gingivitis, which constitute one of the most common causes of tooth loss.
Periodontal diseases
Among the main and most common periodontal diseases is gingivitis. Gingivitis consists of redness, bleeding, and inflammation (swelling) of the gums. This can be caused by multiple factors such as poor oral hygiene (accumulation of bacterial plaque), smoking, poor diet, poorly adhered dental restorations, immunosuppressive diseases, genetics, medications, hormonal changes, etc. Untreated gingivitis can develop into gum disease and spread to the underlying tissue and bone causing Periodontitis, a much more serious disease that can lead to tooth loss. Another common periodontal disease is gingival recession or gum recession, a situation in which the gingival margin moves from its normal position towards the root of the tooth, leaving part of the surface exposed, causing hypersensitivity associated with dentin exposure.
Services and treatment
In our clinic, we have highly qualified periodontists and state-of-the-art equipment for the treatment of periodontal diseases. Treatment will depend on the type of disease and its progression. For the treatment of periodontal diseases, we have available for our patients:
- Initial diagnosis in the mouth with the use of a periodontal probe and review of medical and dental history
- Dental X-ray
- Deep dental cleaning with ultrasonic scaler
- Surgical cleaning to remove bacterial plaque or supra and subgingival tartar
- Gum trimming or gingivectomy with an electrical scalpel
- Mucogingival surgery: making flaps and grafts, etc.
- Bone tissue regeneration

Oral Surgery
What is oral surgery?
Oral surgery is a medical-surgical specialty of dentistry that covers the diagnosis and surgical treatment of diseases of the oral cavity (i.e., teeth, mucosa, and accessory tissues). Depending on the type and degree of difficulty of the surgery, it can be performed by a dentist, a periodontist, an oral and maxillofacial surgeon, or another specialist.
Interventions in oral surgery
There are multiple interventions that can be performed in oral surgery depending on their degree of complexity. We have available for our patients:
- Exodontia or simple extraction: Extraction of a dental piece that has already erupted (i.e., which is visible).
- Surgical extraction of impacted teeth: Extraction of a tooth that has not partially erupted or has not erupted.
- Dental implant: Positioning of a dental implant in the maxillary bone to carry out rehabilitation treatments (crowns, fixed bridges, etc.) in cases of loss of one or more teeth.
- Pre-prosthetic surgery: Preparation of hard and soft tissues (i.e., bone and gum) for the placement of dental prostheses.
- Upper, lower, or lingual lip frenectomies: Correction of the upper lip frenum to close gaps, correction of the lower lip frenum to treat gingival recessions and correction of the lingual frenum to avoid pronunciation and feeding problems due to inadequate mobilization of the tongue.
- Gingivectomy: Design and trimming of the gums when they have suffered a notable thickening because of gingivitis (inflammation or infection).
- Gingivoplasty: Design and trimming of the gums for cosmetic purposes to improve the appearance of the smile.
- Extraction of odontogenic cysts or non-tumor lesions: Extraction of cysts resulting from impacted teeth or prolonged infections in the bone and tooth.
Post-surgery recommendations
Oral surgeries are outpatient with a short recovery period. After the procedure you may experience some type of inflammation and mild discomfort that are part of the normal healing process. Here are the main recommendations to keep in mind:
- Apply cold compresses to the affected area to reduce inflammation.
- Avoid smoking and drinking alcohol.
- Rest according to recommendations and avoid physical exertion.
- Take the medication as directed by the specialist. If any antibiotic treatment has been prescribed, it must be completed, even if the symptoms have disappeared.
- Eat soft foods or a liquid diet according to the specialist’s recommendations.
- Do not consume dairy drinks.
- Keep your head elevated (sit or use pillows) to prevent swelling.
Progressively restore oral hygiene habits: Do not rinse your mouth or brush your teeth in the first hours after surgery or until the specialist tells you to. Subsequently, you can begin to rinse and brush gently, avoiding the area of surgery.

Dental assessment or diagnosis
The main oral diseases are preventable: education, preventive care and the promotion of healthy habits are a very effective strategy and much less expensive than rehabilitation. For this reason, we place great emphasis on the importance of periodically visiting the dentist to carry out an oral health evaluation, prophylaxis, and fluoride application. These are all preventive measures to diagnose the appearance of any disease early and mitigate its long-term impact.
It is important to visit the dentist periodically to carry out a complete assessment and diagnosis of oral health. It is recommended to do it every six months. Similarly, this assessment is mandatory before starting any dental treatment, whether cosmetic or functional, because a detailed assessment of the patient’s oral conditions must be done to define the treatment plan to follow.
We offer complete dental assessments or diagnosis that include:
- General evaluation: detailed examination of the mouth, condition of the teeth and soft tissues such as the tongue, lips, cheeks, palate, and salivary glands.
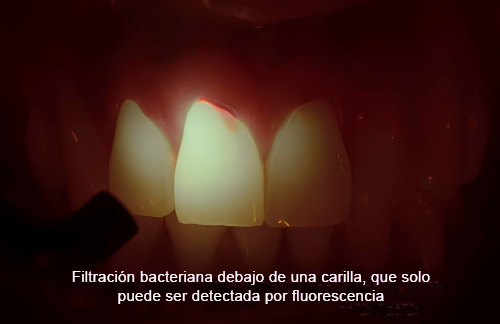
- Detection of cavities with fluorescence: an early and accurate diagnosis of hidden or early-stage cavities (which are imperceptible to the naked eye) is conducted using Facelight fluorescence technology.
- Dental charting: needed for dental fillings, sealants, mismatched dental fillings, fissures, missing teeth, etc.
- Periodontal examination: review of the state of the gums.
- Occlusal exploration: review of the state of the bite, wear on the teeth, bruxism, etc.
The assessment can be accompanied by diagnostic aids such as x-rays or compilation of the patient’s information in the medical history.
Dental prophylaxis or professional teeth cleaning

Dental prophylaxis is a preventive treatment carried out in the dental office, which objective is to eliminate bacterial plaque and dental calculus along the gingival line and interdental areas. Dental prophylaxis is recommended every six months. Dental prophylaxis carried out by our professionals consists of several phases:
- Mechanical removal of bacterial plaque found under the gum and between the gum and teeth, using a Woodpecker ultrasonic scaler that works at high speed, reducing sensitivity in our patients by up to 80%.
- Use of Facelight fluorescence technology to identify points where there may still be bacterial plaque.
- Cleaning of interdental spaces with dental floss.
- Brushing and polishing the teeth using a high-speed brush and prophylactic toothpaste.
- Removal of stains with SandBlaster using water, air, and pressurized sodium bicarbonate.
Fluoride application

Fluoride is a mineral that strengthens dental enamel, preventing damage caused by bacteria and food debris. The presence of fluoride on the surface of the teeth reduces the solubility of the enamel, giving it greater hardness and making it more resistant to the effects of acids and dental cavities.
Currently, all toothpastes have fluoride to facilitate its daily application to the teeth. However, the application of fluoride in the dental office is recommended to enhance its effect.
We carry out the application of fluoride in two modalities:
- Fluoride in Varnish: Concentrated topical fluoride containing 5% sodium fluoride. It is applied to each tooth with a brush, ensuring prolonged contact with the dental enamel.
- Fluoride in buckets: This procedure is done at home. Customized trays are designed for each patient in which fluoride gel is applied. It is recommended to use it for 2-3 hours for 5 days.
It is important to consider that fluoride must be applied in the indicated concentrations, since its excess produces dental fluorosis. Symptoms of dental fluorosis include white, yellow or brown stains on the enamel.
Bruxism
What is it?
Bruxism is an involuntary movement of the jaw in which the teeth rub, slide, or hit each other. Bruxism can happen during the day, but it happens especially at night. In some people, bruxism can be asymptomatic, but it can also cause discomfort such as jaw, neck, and ear pain due to the pressure and force exerted. In addition, temporomandibular joint problems, anxiety, tooth sensitivity and sounds caused by teeth hitting each other, can cause sleep problems (e.g., waking up during the night).
What problems can it cause to my teeth?
Bruxism can cause severe wear of the teeth, leading to fractures or fissures that result from repetitive movements and the force exerted. The wear of the dental pieces produces malocclusion due to changes in the morphology of the teeth, causing other problems such as dental hypersensitivity due to dentin exposure.
What is the indicated treatment?
An initial diagnosis should be made as part of a comprehensive treatment for bruxism. In simple cases, where there is no evident damage or dental wear, the treatment may consist of orthodontics or the use of a muscle-relaxing plate. As the name indicates, this plate works by receiving the bite force of the patient, relaxing the muscles of the face, head and neck, relieving tension in the jaw and reducing discomfort, while protecting teeth from wear. The muscle relaxant plate is custom designed for each patient based on a dental impression. It is made of transparent acrylic resin, so that it can be adjusted to the upper arch without restricting speech or breathing. It is recommended to use it during the day, but especially at night.
In moderate and/or severe cases, where there is wear of the dental tissues, the complete rehabilitation of all the worn dental pieces must be carried out. Treatment could also be accompanied by an orthodontist, head and neck physiotherapist, chiropractor, and/or psychologist. From our field of action in dentistry, the use of a muscle-relaxing plate is recommended to prevent the advancement of bruxism and, in specific cases, the application of Botox to the masseter muscles might be recommended.



Cra 40b # 5b-15
ALMASUR Centro Profesional
Cali – Colombia

